It is fairly common in hospital documentation (especially ICU ward round notes to see references to a patient’s ‘trajectory’.
What is this? Well, it basically reflects whether a patient is getting better, worse, or staying the same.
If we imagine three patients with UTI, appendicitis, and pneumonia, and plot severity of illness versus time on a graph, we might get something like this:

Looking solely at the hospital setting, time starts when a patient comes through the ED doors. With assessment the ED team (hopefully) figures out how sick they are, and what their projected clinical course is. These two functions represent the trajectory, and determine many things:
- WHERE in ED the patient is managed (resus, monitoring, acutes)
- WHO is managing them (both doctor and nurse) and what the staff:patient ratio is
- FREQUENCY of observation, for example vital signs or medical review
- LEVELS OF interventions and investigation – IV cannulae, cardiac monitoring etc
- TIME to more specialised investigation, for example radiology
Speaking from personal experience, it is common for a patients’s initial trajectory to be wrongly estimated.
If the trajectory is OVER-estimated, de-escalating care appropriately is easy – (send ICU away, move patient out of resus etc).
Escalating care appropriately when a patients’s trajectory has been UNDER-estimated is far more difficult. There are multiple barriers, and as such these patients are exposed to risk:
- The patient is often in a clinical environment where their deterioration has been unnoticed for some time (in a 6 bedded ED acutes room on a busy shift, for example). By the time they are identified as deteriorating they are often a fair way into the downward spiral
- Basic investigations and interventions are often incomplete (group and save, relevant blood work, VBG, ECG, good IV access…)
- Escalating their care involves moving them to a new location, which is often difficult. Space in resus or a monitored area may need to be generated, and this takes time if the ED is at full capacity, and often requires convincing another individual (ED supervisor, charge nurse) that your patient needs escalation
- Escalating care often generates angst from other services who are required to be involved in a hurry (does “This patient has been in ED for 3 hours and you’re only phoning me now?!?” sound familiar?)
- There is sometimes shame and embarrassment (whether justified or not) if an ED doctor and/or nurse has incorrectly assessed a patients’s trajectory
- Cognitive errors due to anchoring or fixation may occur (“their mechanism wasn’t bad, and their vitals were normal before, so this must be some sort of problem with the monitor”)
- There is a temptation to bow to space and resource constraints and continue to sort them out in the same environment (“yes, they are worse, but we can still sort them out here”) – the effect of this is that EVERY part of their subsequent assessment and management is slower, and the team feels as though they are continually ‘behind the 8 ball’ (does the ‘Dance of Doom’: acutes–>monitored–>resus–>ICU sound familiar?)

Oh dear…!
With this in mind, having an accurate idea of a patient’s trajectory shortly after their arrival in ED is critical, and yet (unless a patient goes straight into resus) the ED part of trajectory assessment is often determined by a 2 minute triage process! (No disrespect to triage nurses is intended here, they do an amazing job under often adverse circumstances, but triage by definition is a rapid assessment that is inevitably inaccurate on occasion)
THE PREHOSPITAL PHASE IS CRITICAL TO MAKING A PATIENT’S INITIAL TRAJECTORY ASSESSMENT ACCURATE
There are multiple ways in which prehospital care providers and ED staff can work together to make a patient’s initial trajectory assessment as accurate as possible.
1) Pre-hospital notification
The decision as to whether to make a pre-hospital notification call (in NZ this is known as an ‘R40’) is often not black or white – after some experience in the prehospital setting I have been surprised at how tricky this apparently simple decision can be. Putting through an R40 has a HUGE impact on the patient’s assessment and management at the receiving end. With trauma, for example, EDs tend to have two responses and no middle ground – into resus for a full sort-out, or into acutes to take their place in the (often long) queue of ATS category 3 patients. An R40 is often the deciding factor.
For the sake of example, imagine a patient from a moderate speed MVA with a sore chest, stable vitals, a cervical collar in situ, and looking pretty well. With an R40 placed, that patient will probably go into resus on arrival, have a rapid ED assessment +/- trauma call, rapid trauma views and FAST scan, and any advanced imaging will be expedited because the patient is in resus. The same patient without an R40 would be assessed at triage, and if looking well would sometimes be directed to the acutes area. This results in less frequent vital signs, a delay to assessment by a doctor, vastly slower diagnostic imaging, and in the event of a deterioration the barriers to escalation listed above would come in to play.
My suggestion to prehospital providers (and what I do when I am working in the prehospital setting) is, if you have a ‘grey area’ patient and are actually weighing up between doing an R40 and not doing one, just do it anyway! On behalf of ED, we would rather the threshold is low, because it is much easier to de-escalate care than escalate it. Even if a patient is triaged to the acutes area (not resus) after an R40, the patient is still mentally ‘tagged’ by the ED supervisor and charge nurse as potentially needing a closer eye than they would otherwise have got. Don’t underestimate the effect of an R40!
2) Ongoing patient assessment in the prehospital phase
St John and Westpac Helicopter paramedics are very good at repeatedly documenting vital signs while they have a patient in their care. Changes over time are expressed in the ‘Trends’ section of the MIST-AMBO handover, and trends showing deteriorating vitals are arguably the most important part of the handover. While changes in vitals signs may not have a major impact on the care delivered in the prehospital setting, they have a massive impact in ED, especially when identified prior to a catastrophic deterioration. Be sure to place a LARGE emphasis on any concerning trends to the ED team leader. Prehospital providers may need to do this more than once, ED team leaders are often not as calm internally as they appear externally…
3) Keep in mind that investigations that do NOT alter prehospital management will STILL have a significant downstream effect
The classic example of this in current paramedic use if the prehospital ECG. It doesn’t make much difference to how a paramedic manages the patient, but if a STEMI is identified prehospital and a notification made before the patient arrives in ED, the door to PCI time is considerably reduced.
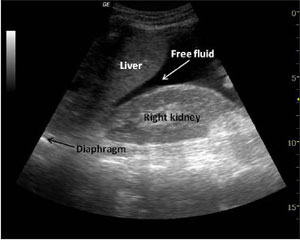
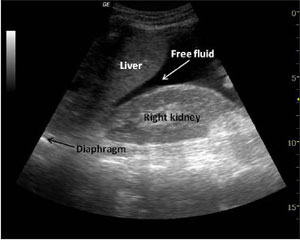 Prehospital ultrasound has a major role to play in the same way. In the setting of trauma, a postive prehospital FAST scan may, for example, mean the patient is met in resus by the trauma consultant while an OR is being made ready, instead of the trauma team being represented in resus by the junior surgical registrar (Note – no disrespect is meant towards junior registrars here, we have all been there!) Minh Le Cong recently tweeted about a patient who had an in-flight scan demonstrating a ruptured ectopic pregnancy. ED was bypassed and the patient went straight to threatre – the ultimate in streamlined care!
Prehospital ultrasound has a major role to play in the same way. In the setting of trauma, a postive prehospital FAST scan may, for example, mean the patient is met in resus by the trauma consultant while an OR is being made ready, instead of the trauma team being represented in resus by the junior surgical registrar (Note – no disrespect is meant towards junior registrars here, we have all been there!) Minh Le Cong recently tweeted about a patient who had an in-flight scan demonstrating a ruptured ectopic pregnancy. ED was bypassed and the patient went straight to threatre – the ultimate in streamlined care!
I am aware that there is some healthy skepticism among paramedics regarding ultrasound use prehospital, and I am certainly not advocating that they defer their usual interventions or prolong the prehospital phase, but if in the future they gain ultrasound skills they will acquire a lot more influence on the patient’s downstream care.
(I would also LOVE to see point of care blood gas machines in the prehospital setting – I frequently use acid/base and lactate to risk-stratify my patients – but this may be a step too far…)
4) Use of technology to convey additional information
 Smartphones are now almost ubiquitous, and some prehospital providers have started taking photographs of prehospital scenes, wounds etc. This is very helpful for the ED team! As an example, I recently looked after a patient from a moderate to high speed MVA. He had an obvious significant limb injury, and was complaining of MILD chest and back discomfort, but appeared clinically well and was haemodynamically stable with normal trauma views. We were weighing up whether to perform a chest/abdo/pelvis CT, and after seeing the pictures of the scene that one of the paramedics had taken (revealing unrecognizable vehicles and a patient literally centimetres from death!) on an iPhone, we elected to perform the scan. We found multiple unsuspected injuries, which had the potential to make the patient unstable in theatre while his limb was being operated on. Without the additional prehospital information proved by the scene photos, we may have elected not to perform the scan.
Smartphones are now almost ubiquitous, and some prehospital providers have started taking photographs of prehospital scenes, wounds etc. This is very helpful for the ED team! As an example, I recently looked after a patient from a moderate to high speed MVA. He had an obvious significant limb injury, and was complaining of MILD chest and back discomfort, but appeared clinically well and was haemodynamically stable with normal trauma views. We were weighing up whether to perform a chest/abdo/pelvis CT, and after seeing the pictures of the scene that one of the paramedics had taken (revealing unrecognizable vehicles and a patient literally centimetres from death!) on an iPhone, we elected to perform the scan. We found multiple unsuspected injuries, which had the potential to make the patient unstable in theatre while his limb was being operated on. Without the additional prehospital information proved by the scene photos, we may have elected not to perform the scan.
5) Improving prehospital to ED handover processes
Even for a relatively short prehospital phase, prehospital providers will have spent far more time with the patient than a triage nurse will. They will be aware of circumstances leading to the request for an ambulance or helicopter (mechanism of injury, for example), have performed an initial clinical assessment, and (perhaps more importantly) will have observed trends over time. They will also have their own clinical ‘gestalt’ or ‘gut feelings’ regarding how unwell a patient is.
Conveying the prehospital assessment of a patient’s trajectory to ED can be challenging
If prehospital staff are handing a patient over at triage or in an acutes area, (without a prehospital notificaton call) they will typically be dealing with a nurse who has multiple competing priorities. Spending 5 minutes with a triage nurse on a Friday evening should convince even the most hardened skeptic of this!
If handover is occuring to a team in resus, there are STILL multiple barriers to important information being conveyed. The resus team is often still being assembled when the prehospital crew deliver and handover their patient, and this generates movement and noise. Right from the start of a resus (before patient arrival) the team leader has a high cognitive load involving clinical management, personnel management, logistics, and generating/maintaining momentum, and putting this aside temporarily to devote enough attention to pick up all relevant detail in a handover can be challenging. Also, of course, there is the fact that ED staff have short attention spans and want to be DOING something – if the patient is put on the resus bed prior to the handover, ED staff CANNOT restrain themselves…
Strategies for improving information transfer are discussed here, and below is a video made by Auckland HEMS (with assistance from St John) demonstrating a structured handover and use of a whiteboard:
Prehospital staff should also feel free to offer their ‘gut feeling’ to the staff they are handing over to. If someone with a bit of experience says to an ED doctor “his numbers are ok but he looks pretty s$%# and I have a bad feeling..” they are guaranteed to get attention! ED doctors have a healthy respect (usually acquired the hard way) for bad ‘gut feelings’.
As one final message – ‘Silos’ need to be broken down

Who needs broken silos when you can decorate them instead?
This particular phrase has a lot of traction among hospital management at the moment, and while some hardened skeptics will dismiss it as ‘MBA wafflespeak’, I think it is actually critical to patient care. The advent of Auckland HEMS seems to have gone some way towards achieving this, as discussed in this post, and more communication and collaboration between healthcare services can only be good for our patients. Working in the prehospital setting has not only taught me new skills (mostly learnt from my paramedic colleagues), but has provided me with a new perspective on EDs and the risks to patients that come from current systems.
Personally I would welcome more paramedic presence in ED, both in training and at post-graduate level. Paramedics already play a critical role in patient care, but I wonder if they realise quite how significant an impact their patient assessment and handover communication has on a patient’s downstream care in an imperfect, frequently overloaded hospital system?
 Let it never be said that New Zealand’s own medical journal does not bring you the latest in ground-breaking research and innovation:
Let it never be said that New Zealand’s own medical journal does not bring you the latest in ground-breaking research and innovation: